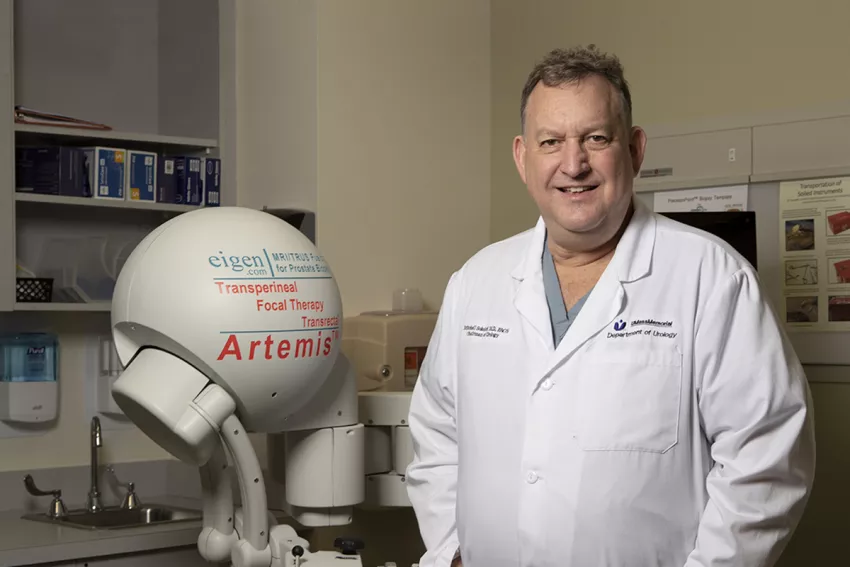
Photo above: Mitchell Sokoloff, MD, with the Artemis 3D Semi-Robotic Prostate Fusion Biopsy System, part of a suite of advanced treatments and techniques the UMass Memorial Medical Center Urology team offers patients. (Photo credit: Matt Wright.)
Lovo Koliego, MSN, RN, heard of Mitchell Sokoloff, MD’s, advocacy for prostate screening as she searched for a speaker to address the subject at a community event in Worcester, MA – and with that, a new health promotion partnership was born.
The tip came from nephrologist Maria DelRosario, MD, a colleague of Koliego’s on UMass Memorial Medical Center’s kidney and liver transplant, GI and dialysis unit. In addition to her nursing career, Koliego founded Community Health Awareness Network (CHAN), a nonprofit that empowers immigrant communities through outreach and access to high-quality, culturally sensitive care. CHAN’s efforts to reduce health care disparities include collaborations with local experts on educational programs.
“I have learned that immigrant men are often uncomfortable discussing prostate issues with a female, so I needed a way to get in front of them more broadly in the community by connecting them with a male,” said Koliego, herself an immigrant from Liberia. “Dr. Sokoloff was my first outreach for this purpose, and we have worked together since.”
PASSION FOR HEALTH
The busy Koliego – a 2022 Leadership Worcester alumna, Commission on Elder Affairs board member and Women’s Initiative Diversity Equity and Inclusion (DEI) committee member – has worked to ensure immigrants can navigate the health care system, building their knowledge of available services and practitioners, as well as their confidence when accessing them. “I have a passion for the health of my community,” Koliego said.
Enter Sokoloff, founding chair of the Department of Urology at UMass Memorial Medical Center, and Professor, UMass Chan Medical School, whose commitment to community health is equally deep-seated. Koliego and Sokoloff present information to men of West African or Afro-Caribbean descent – typically at local churches, after services or breakfasts – to educate them about a disease of particular risk to them: prostate cancer.
“Prostate cancer is the second most common type of cancer in American men, and one in six men will receive a prostate cancer diagnosis in their lifetime,” said Sokoloff, who is an expert in the management of high-risk, locally advanced and recurrent prostate, kidney and testis cancers. “But African American men are 1.6 times more likely to be diagnosed with prostate cancer than white men.”
AT HIGH RISK
Prostate cancer’s genetic profile in African Americans and Black immigrants from West Africa and the Caribbean results in a more aggressive form of the disease, according to Sokoloff. And in many cases, the cancer is diagnosed at an advanced stage due to factors that hinder early screening, such as difficulty in accessing care, lack of insurance coverage or misunderstandings about treatment.
Increasing the number of men undergoing routine prostate screenings, and at a younger age, is vital because early-stage prostate cancer usually has no symptoms. When a weak urine stream, painful or frequent urination, blood in urine or semen, or discomfort in the pelvic area occur, advanced prostate cancer may be present and uncurable.
COMPREHENSIVE PROSTATE CARE
Sokoloff has led or been a part of surgical urologic oncology teams at the University of Arizona College of Medicine –Tucson, Oregon Health & Science University and UChicago Medicine. He joined UMass Memorial in 2014 to establish the clinical system’s urology department, re-establish the urology residency program and foster research activities of current and future faculty members at UMass Chan Medical School.
“The opportunity to start a program from scratch is rare in academic settings – that drew me here,” Sokoloff said. “Developing a fellowship-trained faculty, with tertiary specialization – such as oncology, stones, reconstruction and voiding dysfunction – and training programs for medical students and residents has offered a unique academic nature of practice, with a phenomenally multidisciplinary team of urology specialists providing comprehensive services to our patients.”
This program is essential for addressing another unique factor here: “Worcester County has the highest rates of prostate cancer incidence and deaths in Massachusetts. State data suggest that our program has reduced rates since we started,” Sokoloff said. “We continue to recruit faculty and provide outstanding outcomes and quality metrics, including for readmission and length of stay, that are a standard for the community.”
MOST ADVANCED TREATMENTS
Sokoloff recently performed a single-port prostatectomy using a surgical robot. While still rarely performed in New England, this procedure has become the norm for prostate cancer treatment at UMass Memorial.
In addition, the urology team launched one of the first high-intensity focused ultrasound (HIFU) programs in New England, furthering their development of focal therapies for prostate cancer. This complements the advanced fusion biopsy procedure, which combines images from an MRI scan and ultrasound to produce a 3-D portrait of the prostate, allowing the physician to pinpoint an abnormality and guide the biopsy needle or therapeutic probe to its target more effectively.
These techniques, complemented by programs of active surveillance, which applies to many patients; other surgical options; radiation and now focal therapy, which can eradicate small tumors while leaving the rest of the prostate intact; and an array of medications, offer a full spectrum of the newest and most advanced technologies available for prostate cancer treatment. Sokoloff’s and Koliego’s quest in the community is to ensure those at high risk know about this range of care options, with the first step being prostate cancer screening.
MAKING CONNECTIONS

Pastor Stephen Aryitey of Faith Fellowship in Worcester has hosted Sokoloff and Koliego for several years and describes the physician’s approach to his gathered congregations as relatable. “He comes casually dressed and takes out the formality and medical language. He’s an easy speaker as he breaks down information,” said Aryitey, noting that it makes men more receptive to hearing about the topic in a comfortable setting.
Tackling the misperceptions that surround prostate screening and cancer treatment is key, according to Aryitey, as attendees often associate hospitals with pain, suffering and death. “Dr. Sokoloff knows they are concerned about probes and pokes and how these might impact their lives. He demystifies, counters myths and describes the prostate specific antigen (PSA) screening as a piece of cake.”
Incentives like gift cards encourage hesitant listeners to ask questions. And before leaving the event, Sokoloff and Koliego ask for feedback to ensure their messages were received.
Spreading The Word
Sayon Johnson can attest the messages were, indeed, received. Originally from Liberia and a resident of Worcester for 18 years, Johnson attended a Sokoloff presentation after speaking with Koliego. As a result, at his annual physicals, he now makes a point to talk to his doctor about prostate screening.
Like Pastor Aryitey, Johnson also spreads the word among his friends and neighbors. With the knowledge he gained from Sokoloff, Johnson advised a friend who was making frequent trips to the bathroom at night to speak to his doctor. It turned out the friend needed prostate treatment.
“I plan to mention the presentations to the men who gather after soccer practice,” said Johnson, a service coordinator for the Massachusetts Department of Developmental Services, who is skilled at connecting with people where they are. “I say, ‘just come and listen.’ Some hesitate because they fear learning they have cancer, or that if they get treatment, it will ruin their sex lives.”
But, he added, “many don’t know their family medical history, and as they learn about the symptoms, some realize their dad might have had prostate cancer. Learning that it’s inheritable helps [men to take the next step toward screening]”.
HAVING AN IMPACT
Since Sokoloff began his partnership with Koliego in March 2019, “we’ve seen the impact in people coming to see us,” he said. “Fortunately, with the advanced technology and medication available, many men who receive a prostate cancer diagnosis can live long lives with it.”
Next, Koliego is adding an outreach effort she calls the barbershop project, educating men at a prime location, as she continues to promote the in-person and online presentations Sokoloff provides. “I love his presence in the community. He never hesitates. Education is key – the more people take the time to explain, the more people will understand.” And she has a message for practitioners: “Preventive care like screening is huge; take one or two minutes to talk to your patients!”